Upper GI
4. GERD and PUD
1. Gastroesophageal Reflux Disease (GERD)
Pathophysiology
- GERD occurs due to dysfunction of the lower esophageal sphincter (LES), resulting in retrograde flow of stomach contents into the esophagus.
- Key contributing factors:
- Transient LES relaxations.
- Hiatal hernia.
- Impaired esophageal motility.
- Delayed gastric emptying.
Clinical Features
- Typical Symptoms:
- Heartburn (burning retrosternal discomfort).
- Acid regurgitation.
- Atypical/Extra-esophageal Symptoms:
- Chronic cough, asthma, laryngitis, non-cardiac chest pain.
- Alarm Symptoms:
- Dysphagia, odynophagia, weight loss, GI bleeding (indicative of malignancy or complications).
- Note: Reflux itself does not typically cause odynophagia—investigate for infections such as HSV, CMV, or candidiasis.
Diagnostic Approach
- Clinical Diagnosis: Typical symptoms with response to PPI trial.
- Endoscopy:
- Indicated in patients with alarm symptoms or PPI-refractory GERD.
- Assess for erosive esophagitis, Barrett’s esophagus.
- Los Angeles (LA) Classification for Erosive Esophagitis:
|
Grade |
Endoscopic Findings |
|
A |
Mucosal break ≤ 5 mm that does not extend between folds |
|
B |
Mucosal break > 5 mm but does not extend between folds |
|
C |
Mucosal break continuous between folds, < 75% of circumference |
|
D |
Mucosal break involving ≥ 75% of the esophageal circumference |
- Surveillance Recommendation:
- Recommended only for patients with grades C or D esophagitis after 6–8 weeks of PPI therapy.
- Routine surveillance not recommended for LA grades A or B.
- Esophageal pH Monitoring (± Impedance):
- Confirms GERD in endoscopy-negative cases.
- Useful in atypical symptoms or prior to surgical interventions.
- Demeester Score Components:
- Supine reflux episodes.
- Upright reflux episodes.
- Total reflux duration.
- Number of reflux episodes.
- Episodes > 5 minutes.
- Longest reflux episode.
- Interpretation: A Demeester score > 14.72 indicates pathological acid reflux.
- High-Resolution Manometry (HRM):
- To evaluate for esophageal motility disorders.
Management
- Lifestyle Modifications:
- Weight loss, head-of-bed elevation, avoidance of late meals, trigger foods.
- Pharmacological Treatment:
- First-line: Proton pump inhibitors (PPIs) (e.g., omeprazole) for 8 weeks.
- Second-line: H2 receptor antagonists or PPI dose adjustment.
- Surgical Intervention:
- NICE Recommendations: Consider laparoscopic fundoplication for patients with:
- Confirmed acid reflux and adequate symptom control with PPIs but preference for surgical management.
- Confirmed acid reflux with PPI-responsive symptoms but intolerance to long-term acid suppression therapy.
2. Peptic Ulcer Disease (PUD)
Pathophysiology
- Definition: Mucosal defect in the stomach or duodenum due to an imbalance between protective factors (mucus, bicarbonate, prostaglandins) and harmful factors (acid, pepsin).
- Aetiology:
- Helicobacter pylori infection.
- NSAID use (inhibits prostaglandin synthesis).
- Zollinger-Ellison syndrome (gastrin-secreting tumor).
Clinical Features
- Gastric Ulcer:
- Epigastric pain worsens with food.
- Associated with nausea, early satiety.
- Duodenal Ulcer:
- Epigastric pain relieved by food or antacids.
- Pain recurs 2-3 hours postprandially or at night.
- Complications:
- GI bleeding (melena, hematemesis).
- Perforation (acute severe abdominal pain).
- Gastric outlet obstruction.
Diagnostic Approach
- Endoscopy:
- Gold standard for visualizing ulcers.
- Biopsy indicated to rule out malignancy (especially for gastric ulcers).
- H. pylori Testing:
- Culture of Gastric Biopsy: Sensitivity ~72%.
- Rapid Urease Test: 80-95% sensitivity, 95-100% specificity.
- Histology: 80-90% sensitivity, 95% specificity.
- Urea Breath Test: 95% sensitivity, 98-100% specificity.
- Serology (IgG antibodies): Indicates past infection—potentially useful when PPIs cannot be stopped.
- Note: Gastric biopsy results can be false negative following PPI treatment.
- Post-treatment eradication confirmation: Urea breath test or stool antigen test (both indicate active infection).
Impact of Eradication Therapy
- Duodenal Ulcers:
- Slightly increases healing (5.4% additional benefit over acid suppression alone).
- Significantly decreases recurrence (52% more patients ulcer-free at 12 months).
- Gastric Ulcers:
- No significant effect on healing.
- Reduces recurrence (32% more patients ulcer-free at 12 months).
- NSAID-induced Ulcers:
- No significant effect on healing when NSAIDs are continued.
- Continued NSAID use markedly reduces the benefit of eradication therapy on recurrence.
Zollinger-Ellison Syndrome (Gastrinoma)
- Presentation: Multiple duodenal ulcers, refractory to PPI treatment, and possible diarrhea.
- Diagnostic Steps:
- Endoscopy (OGD): Identifies multiple or PPI-resistant duodenal ulcers, possibly enlarged gastric folds.
- Low Gastric pH (<2) despite PPI use.
- Fasting Gastrin > 1000 pg/mL (10x upper limit of normal).
- If gastrin < 1000 pg/mL: Perform a Secretin Stimulation Test (off PPI if possible, except in severe cases).
- Imaging for Localization:
- CT, MRI, or radio-labeled somatostatin scintigraphy.
- Endoscopic ultrasound (EUS) for detecting small tumors.
- Chromogranin A: Less sensitive than gastrin and can be falsely elevated with PPI use.
- Differential Diagnosis: Antral G-cell hyperplasia (poor response to secretin test, no tumor on imaging).
- Association: Look for MEN1 syndrome (parathyroid, pancreatic, and pituitary tumors).
- Treatment:
- PPI Therapy: High-dose to control acid secretion.
- Octreotide: Consider if PPI therapy is inadequate.
- Localized Tumor: Surgical resection (especially in MEN1 with multifocal tumors).
- Metastatic Disease: Liver resection or embolization; consider octreotide.
Management
- Lifestyle Changes:
- Avoid NSAIDs, smoking, alcohol, and stress.
- Pharmacological Therapy:
- First-Line H. pylori Eradication (7-Day BID Therapy):
|
Scenario |
Regimen |
|
First-Line |
PPI + Amoxicillin + Clarithromycin |
|
Alternative First-Line |
PPI + Amoxicillin + Metronidazole |
|
Penicillin Allergy |
PPI + Clarithromycin + Metronidazole |
|
Pen Allergy, Prior Clari |
PPI + Bismuth + Metronidazole + Tetracycline |
- Second-Line Therapy:
- No penicillin allergy: PPI + amoxicillin + clarithromycin/metronidazole (whichever was not used first-line).
- Previous exposure to clarithromycin and metronidazole: PPI + tetracycline (or levofloxacin if tetracycline cannot be used).
- Penicillin Allergy:
- No prior quinolone exposure: PPI + metronidazole + levofloxacin.
- Prior quinolone exposure: PPI + bismuth + metronidazole + tetracycline.
- NSAID-induced ulcers:
- Discontinue NSAIDs and initiate PPIs for 8-12 weeks.
- Consider prophylaxis with PPIs for high-risk NSAID users.
- Surgical Intervention:
- Reserved for complications such as perforation or refractory bleeding.
References
- NICE CG184 – GERD and Dyspepsia Guidelines.
- Lyon Consensus. Modern Diagnosis of GERD Accessed online.
- ESGE Guidelines for PUD Management ESGE 2019.
Images:
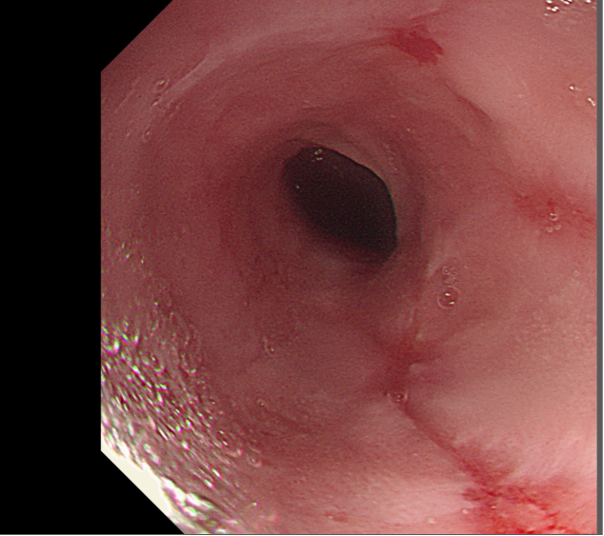
Figure 1: Reflux oesophagitis.